Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-6003
Review Article(ISSN: 2638-6003) 
Best Position and Duration for Immobilization in Primary Anterior Shoulder Dislocation: A Systematic Review and Meta-Analysis of Randomized Controlled Trials Volume 5 - Issue 1
Dharmesh Patel*, Avtar Singh, Rajeev Vohra and Sandeep Chauhan
- Senior Resident, MBBS, DNB (Ortho), University Amandeep Hospital, India
Received:February 05, 2021; Published:February 23, 2021
Corresponding author: Dharmesh Patel, Senior Resident, MBBS, DNB (Ortho), University Amandeep Hospital, G T road, Model Town, Amritsar, Punjab, India
DOI: 10.32474/OSMOAJ.2021.05.000205
Abstract
Background: Anterior shoulder dislocation is the most common injury of the glenohumeral joint and primarily caused by traumatic event and shoulder instability. Recurrent dislocation of anterior shoulder dislocation is a common occasion following the primary anterior shoulder dislocation. Generally, anterior shoulder dislocations are treated with closed reduction, stages of immobilization, and series of physical exercise treatment. This systematic and meta-analysis study were conducted to consider the best duration and position of immobilization after primary anterior shoulder dislocation reduction to reduce the risk of anterior shoulder dislocation recurrence.
Materials and Methods: PubMed, Cochrane, NCBI, Elsevier were used to searched randomized controlled trials. Two reviewers selected studies for inclusion, assessed methodological quality, and extracted data. The studies were peer-reviewed by two consultant, then selected based on inclusion criteria.
Study Design: Systematic review and meta-analysis; Level of evidence, I, II.
Result: A total of seven randomized controlled trials (635 patients) included in this systematic review and meta-analysis. In these studies, the recurrence rate of instability in ER group was 23.45% (76/324) versus IR group was 33.44% (104/311). Pooled data showed that ER immobilization significantly reduced the recurrence rate of instability (risk ratio, 1.83; P= 0.0001) compared to IR immobilization. Pooled data also summarized that immobilization in 3 weeks significantly reduced the risk of recurrence compared to ER immobilization in 4 weeks (risk ratio, 2.35; P=0.01). The subgroup analysis has been made and there was no significant difference between ER immobilization and IR immobilization in patient aged <30 years (P=0.29). Analysis on 3 studies showed that there was no significant difference in WOSI score between both groups (p=0.32).
Result:Best position and duration for primary anterior shoulder dislocation is ER immobilization in 3 weeks. This study found it significantly reduces the risk of recurrence instability. Furthermore, more studies needed to support the result of our studies to determine best assessment for anterior shoulder dislocation and the risk of recurrence instability.
Keywords: Anterior Shoulder Dislocation; Immobilization; External Rotation; Recurrence Rate; Meta-Analysis
Introduction
The glenohumeral joint has its large arc of motion, making them prone to mild or even severe injury [6,12]. The most common injury to the glenohumeral joint is anterior shoulder dislocation [12], which possibly the cause of a traumatic event or the shoulder instability itself.9 Anterior shoulder dislocation contributes 96% of total shoulder dislocations [11, 19]. The incidence of primary anterior shoulder dislocation is between 11.2 to 26.2 per 100,000 people. Recurrent dislocation is caused by a lesion in the glenoid labrum; the primary stabilizer of the shoulder. The prevalence of primary anterior shoulder dislocation is high in athletic activities, with the mechanism of apprehension position of shoulder abduction and external rotation [29]. Traditionally, anterior shoulder dislocations are treated with closed reduction, stages of immobilization in external or internal rotation for 2-6 weeks, and a series of physical exercise treatment, perhaps reducing the risk of recurrent dislocation and enhance the soft tissue healing [12, 18, 20] Despite its protocol to treat the anterior shoulder dislocation, the most advantageous time and position of immobilization yet the best position has to be proven. Therefore, we conducted a systematic review and meta-analysis from the available literature to consider the best duration and position for immobilization after the reduction of anterior shoulder dislocation.
Materials And Methods
Literature Search
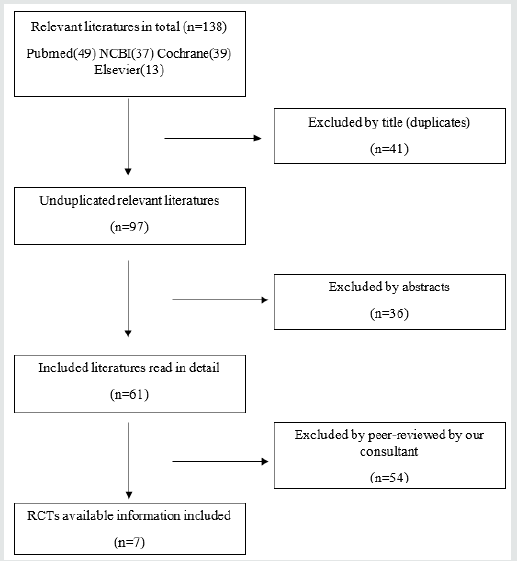
Electronic databases (PubMed, NCBI, Cochrane, and Elsevier) were searched without limit. This study was conducted strictly following the methods established in the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA). We independently reviewed the titles and abstracts and strictly followed the inclusion criteria12: [1] the patient must be diagnosed with primary anterior shoulder dislocation; [2] direct comparison between internal and external rotation immobilization with recurrence rate in result for comparison; [3] more than 1-year follow up; [4] must be randomized controlled trials (RCTs). Exclusion criteria included studies where: [1] retrospective study, case reports, reviews, observational studies; [2] the outcome data were not available; [3] follow up time less than 1 year. Publications were excluded by title review, and abstracts, of all studies that were not excluded by title were reviewed to meet the criteria mentioned above. Then publications that have been reviewed were retrieved in full text and were read in detail.
Data Extraction and Quality Assessment
We reviewed and extracted independently all the studies. Especially year of publication, study design, patient demographics (age, sex, sample size), type of immobilization, duration of immobilization, mean follow-up time, loss to follow up rate, recurrences rate, and WOSI Score. We used data from the analysis of treatment from the available data from the studies. If the data were not reported, we extracted them from the accompanying graphs.
Statistical Analysis
To perform the meta-analysis, we used RevMan version 5.3 software (Cochrane Collaboration). We used the risk ratio (RR) and a 95% CI as a pooled measure for dichotomous data. Inconsistency index [I2] test which ranges from 0% to 100% was used to assess heterogeneity across studies. A value above 50% or P <0.05 indicates statistically significant heterogeneity. We used the Mantel-Haenzsel method with a fixed-effect model for meta-analysis and a random effect model was used in case of heterogeneity. All P values were 2-tailed with a statistical significance set at 0.05 or below.
Source of Funding
No external funding support was received for this study.
Results
The literature search identified 138 studies. Among these 138 studies, 41 were excluded by titles (duplicates), 36 were excluded by abstract. Leaving 61 studies to be screened, and after we reviewed all the studies, we did consult with our consultant and 54 have been excluded by peer-reviewed, leaving 7 RCT in total to be included in our study.
Description of Studies
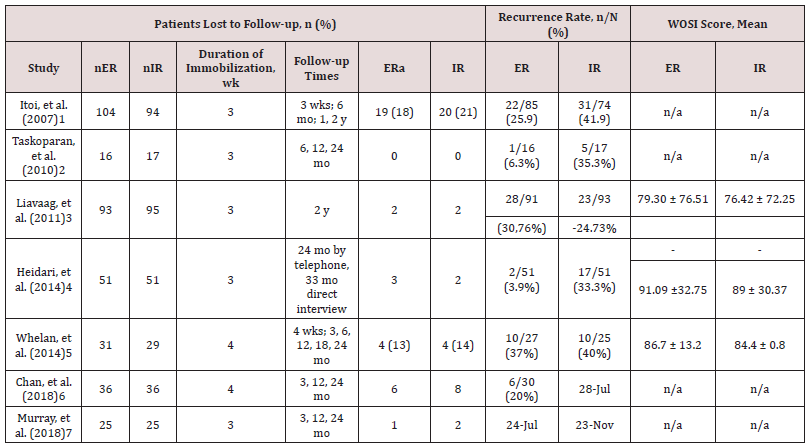
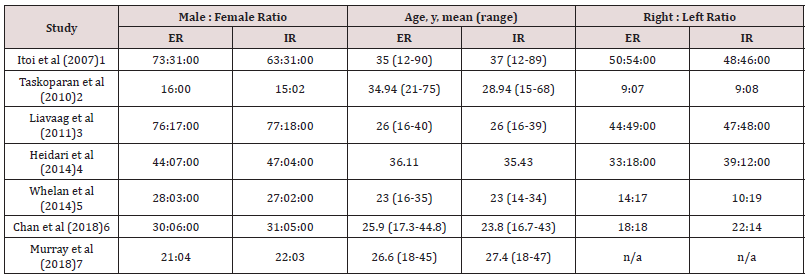
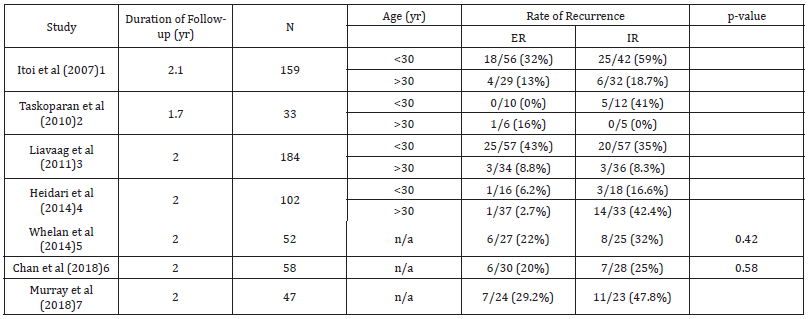
We included 7 RCTs comparing ER and IR immobilization after primary shoulder dislocation. Overall, there were 635 patients included in this study, with a mean age of 29.2 years across the 7 included studies. The overall follow-up time for the included studies was 23.6 months. Male to female ratio was 288:68 in the ER group, and 262:65 in the IR group. Duration of immobilization ranged from 3 to 4 weeks. The characteristics, main outcomes, and patient demographics included in the studies are shown in Tables 1 to 3. Itoi, et al [1] Itoi et al. reported in a clinical trial that immobilization in ER was shown to reduce the risk of recurrence shoulder dislocation compared to the IR groups. There were 198 participants (104 were treated in ER and 94 in IR). The average patient age reported was 37 years. The inclusion criteria included [1] firsttimer dislocation, [2] within 3 days after dislocation, [3] no associated fracture based on radiograph findings. They reported that recurrent dislocation was 25% in the ER group (22/85), and 42% in the IR group (31/74). Taskoparan, et al. [2] performed a randomized clinical trial comparing 3 weeks of immobilization in 10o of external rotation and internal rotation. The inclusion criteria of this study were primary anterior shoulder dislocation, no hyperlaxity of the shoulder, and admission on the first day of reduction after a dislocation. However, the exclusion criteria were not stated in this study, but it was stated that 2 patients were excluded from the study with, respectively, brachial plexus injury and hyperlaxity of the shoulder. A total of 33 met the inclusion criteria with 20 patients who encountered the dominant side. To be noted, 1 from 16 patients (6.3%) in external rotation group and 5 from 17 patients (29.4%) in internal rotation group experience anterior shoulder dislocation recurrence (p>0.05). While patients aged between 21-30 in the ER group did not fall on anterior shoulder dislocation recurrence, 5 patients in the IR group did (p=0.035). Hence, this study showed that external rotation is an effective preference to prevent recurrence of anterior shoulder dislocation rather than traditional internal rotation sling Liavaag, et al. [3] enrolled in a multicenter clinical trial from 13 hospitals, comparing immediate 3 weeks immobilization of both internal rotation; sling and swathe; and 15o external rotation; external rotation immobilizer. The inclusion criteria were [1] patients aged 16 – 40 years old and [2] successful reduction of primary traumatic anterior glenohumeral dislocations which were documented with a conventional radiograph. Furthermore, glenoid fracture with large osseous defect, greater tuberosity fracture with malalignment after repositioning, nerve injury-prone to the dislocation or even the reduction, and the unwillingness or ineptitude to take part in the study were excluded. Afterward, the outcome of the intervention was measured with a minimum of 24 months (2 years) of follow-up after the first anterior shoulder dislocation. A total of 188 patients; 93 randomized to ER and 95 randomized to IR; were acquired in the study with the mean age of 26.8 ±7.1 years old, ranging from 16-40 years old. It was shown that the recurrence rate (primary outcome) of internal rotation immobilization was 24.7% and 30.8% for external rotation immobilization with p = 0.37. Moreover, the secondary outcome measures the Western Ontario Shoulder Instability Index (WOSI) with a median score for the ER group was 238 and 375 for the IR rotation group, the difference was not significant (p=0.32). From the study, it was concluded that immobilization in the external rotation did not reduce the rate of recurrence for patients with primary anterior shoulder dislocation Heidari, et al [4] performed a prospective, randomized, controlled, clinical trial to compare the effectiveness of immobilization in external rotation (15o abduction and 10o external rotation) and internal rotation. The subjects were picked from the ED within 6 hours after the primary unilateral anterior shoulder dislocation, ranging from 15-55 years old and inclining to be followed up. Patients with previous shoulder issues, surgical joint repair, multidirectional instability, shoulder injuries requiring surgical intervention, associated with fractures of the shoulder upon routine radiographic examination, and unwilling to be followed up for the next 24 months were excluded. Afterward, all the patients included were assigned in a ratio of 1:1, respectively, in the adduction – internal rotation (AdIR) group and abduction – external rotation (AbER) group. The primary outcome was a recurrent dislocation, measured with WOSI. From the results, it was shown that the recurrence rate was significantly higher in AdIR group (33.33%) rather than the AbER group (3.9%), with p < 0.001. Hence, the abducted and externally rotated stabilization for primary anterior shoulder dislocation has more benefit in reducing the risk of anterior shoulder dislocation recurrence Whelan, et al. [5] Prospective multicenter randomized control trial with singleblinded evaluations was a study conducted by Whelan et al to 2 study groups. They are external rotation brace (90o elbow flexion, 0o shoulder abduction and flexion, and 0o- 5o external rotation at the shoulder), and internal rotation sling (90o of elbow flexion, 0o of shoulder abduction and flexion, and 70o-80o of internal rotation at the shoulder). Both groups were obligated to wear the fixator for a total of 4 weeks. Furthermore, the exclusion criteria of this study including previous instability of the affected shoulder with significantly associated fractures of the proximal humerus, glenoid, or scapula (except Hill-Sachs lesion and/ or small bony Bankart lesions) or those who were unwilling to participate in the study. The result was 37% (10/27) of ER group experienced recurrent dislocation and subluxation, while 40% (10/25) of the IR group (p=0.41 for recurrent instability between groups). The WOSI scores were not different between the groups respectively 87% and 84% for external rotation and internal rotation (p=0.74). Hence, it was concealed from this study that there was no significant difference in the rate of recurrent dislocation or instability between the groups of external and internal rotation Chan, et al. [6] A prospective, multi-center randomized control trial was conducted by Chan, et al. between 2006 and 2010. This study looked into the better outcome between using the conventional sling/ Polysling (internally rotated shoulder) or external rotation brace (30o externally rotated shoulder and 30o abduction) in the first occurrence of anterior shoulder dislocation for 4 weeks after the incidence. Starting from September 2006, patients with primary anterior shoulder dislocation ranging from 14-45 years old were put into the study. Exclusion criteria included an associated fracture, an indication for surgery (as determined by the recruiting surgeon), inability to provide informed consent, learning difficulties, mental illness, dementia, significant co-morbidities, or if the patient was unwilling to participate. After 24 months, the follow-up data showed that 30% of subjects who were put in internal rotation sling experienced recurrence of anterior shoulder dislocation, while 24% of subjects of external rotation and abduction did come through anterior shoulder dislocation recurrence. From the study by Chan et al, it can be concluded that ER bracing is unlikely more superior to provide advantages in traumatic first-time anterior shoulder dislocation Murray, et al. [7] A report from Murray, et al found that there is no significant difference between the ER and IR groups. Fifty patients were included in the study, which 25 patients allocated in the IR group and others [25] in the ER group. One patient refused to be treated in external rotation, and three patients were lost to follow-up. This study also reported that 38.3% of the patients had recurrent shoulder dislocation within two years. The recurrence rate was 47.8% (11 of 23) in IR group and 29.2% (7 of 24) in the ER group. They also report that in the subgroup aged between 20 and 40 years, the recurrence rate was 50% (9 of 18) in the IR group and 17.6% (3 of 17) in the ER group (p=0.044). For the patient aged under 20 or over 40 years found that no significant difference was found between IR and ER groups.
Recurrence Rates
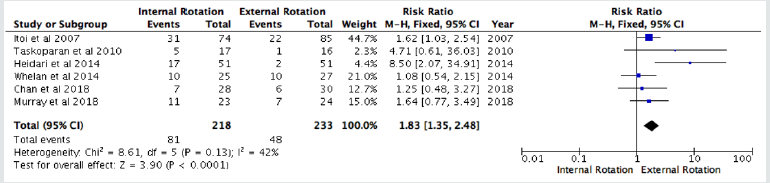
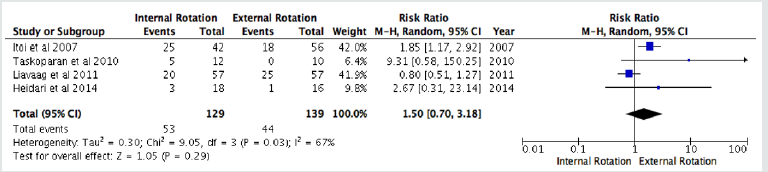
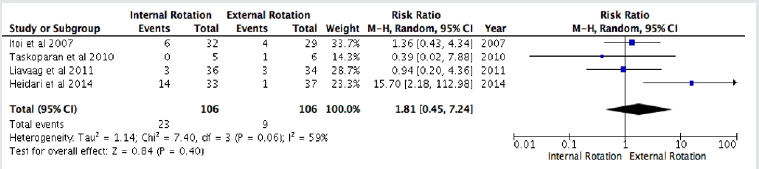
We included 6 studies for the recurrence rate at all ages. All data were pooled to make a meta-analysis. We found that ER immobilization was significantly reduce the recurrence rate at all ages (RR: 1.83 (1.35, 2.48); p=<0, 0001; I2=42%) (Figure 2). Moreover, in sub-group analysis we found no significant difference in recurrence rate based on age, <30 years (RR: 1.50 (0.70, 3.18); p= 0.29; I2=67%) (Figure 3), and >30 years (RR: 1.81 (0.45, 7.24); p=0.32; I2=59%).
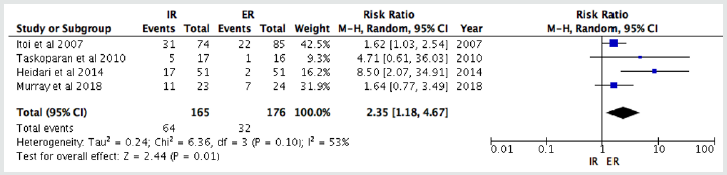
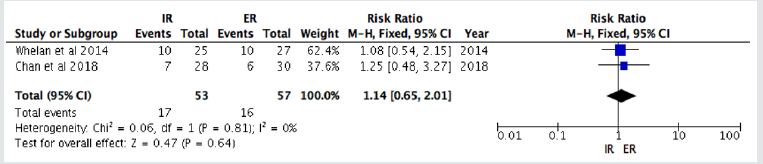
Duration of Immobilization
We included 6 studies for the duration of immobilization which separated into two groups, inclusive of 3 weeks and 4 weeks. We pooled all the data to make a meta-analysis. From the forest plot, we found that 3 weeks of immobilization in ER significantly reduce the recurrence rates (RR of 2.35 (1.18, 4.67); p= 0.01; I2=53%). In contrast, 4 weeks immobilization showed no significant difference to reduce the recurrence rate of anterior shoulder dislocation (RR=1.14 (0.65, 2.01); p= 0.64; I2=0%).
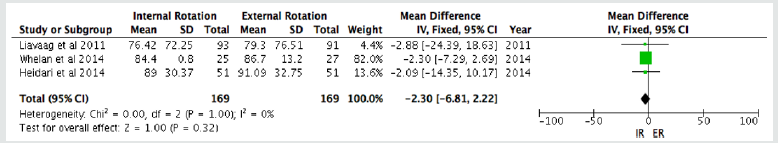
The Western Ontario Shoulder Instability Index (WOSI) Scores
The WOSI scores analysis was obtained from 3 studies to value the disease-specific quality of life (QoL) deficits between both IR and ER groups. It was found that there was no significant difference in the WOSI scores between both groups (p = 0.32, I2 = 0%).
Discussion
Recently, several studies showed reports about preferences in immobilization. Yet its duration, after a primary anterior shoulder dislocation, remains questionable, controversial, and debatable [25]. In our study that includes a meta-analysis of level I and II trials, we added 2 RCTs that had not been included in the previous meta-analysis [6, 7]. We pooled recurrence rates by age (all ages, <30 years, and >30 years) to evaluate the effectiveness of immobilization for reducing the risk of recurrence rate objectively. We also pooled the duration of immobilization of primary anterior shoulder dislocation to conclude the significance duration for reducing recurrence rate, WOSI score also being pooled to evaluate the better immobilization position. The previous systematic review and meta-analysis studies reported that there was no statistically significant difference between ER and IR immobilization to reduce the risk of recurrence [21,31]. In contrast, one of the recently published systematic review and meta-analysis showed that there is a statistically significant difference in recurrence rate based on immobilization, the investigator found that ER immobilization is superior to IR immobilization based on pooled data that has been shown in their study (p = 0.007)8.
The summary of our review and meta-analysis based RCTs with the highest-level evidence (level I or II trials) found that ER immobilization is statistically significant to reduce the recurrence rate (P<0.0001) at all ages, although we did not find any statistically significant difference in group ages <30 years (P=0.29), and >30 years (P=0.40). Even though we found a significant difference between the groups, still more RCTs are needed to prove the efficacy and preferred immobilization position [21]. According to our study, ER immobilization after primary anterior shoulder dislocation was preferably superior to IR immobilization, perhaps reducing the risk of recurrence and shoulder instability [1,17]. It was found no detachable contact force when the arm placed in IR immobilization after anterior shoulder dislocation. ER immobilization has been suggested based on an MRI study which stated that external rotation would maintain the labrum and capsule in close contact to the glenoid and enhance the tension on the subscapularis muscle [19,32]. Moreover, a biomechanical study on cadaver proved that gleno-labral contact was much wider when the shoulder was externally rotated in 450. [2,19,22,32] However, 45o in the external rotation will increase the contact force and seem difficult to be tolerated by the patients, therefore, most of the studies performed 10o external rotation to increase the cooperation rate in immobilization [2,22]. A radiologic study also confirmed that immobilization in external rotation had a positive impact in decreasing the hemarthrosis and reduction of anterior capsule detachment and labral lesions [1, 2, 17, 32]. Regarding to its superiority, some studies also reported the conflicting results on patients’ acceptance to use external rotation brace [23]. In 2010, Paterson, et al made an analysis for preference duration of immobilization in primary anterior shoulder dislocation. 25 The analyst showed that duration of immobilization <1 week and >3 weeks had no statistically significant difference in reducing the risk of recurrence. Since then, no reports have been showing about preferred durations of immobilization of primary anterior shoulder dislocation. Two comparisons had been made in our study to conclude the best duration of immobilization. Pooled data from 3 weeks of immobilization showed a statistically significant difference to reduce the recurrence rate (p=0.01). Otherwise, we found no statistically significant difference in the duration of immobilization in 4 weeks (p=0.64). One of the most common complications of anterior shoulder dislocation is hemarthrosis of the glenohumeral joint which would maintain the anterior capsule detachment.21,28,33 Hemarthrosis itself would resolve and be absorbed only after 3 to 7 weeks, which why 3 weeks are considered as the minimum compliance time of immobilization 21,33.
Conclusion
This meta-analysis study summarized that ER immobilization in 3 weeks is the best position and duration for immobilization after primary shoulder dislocation based on recent RCTs (Level I; II Evidence). We suggest more meritorious and thorough prospective randomized controlled trials with long-term follow-ups to be conducted, perhaps cutting off the biases in meta-analysis study and annotate an objective outcome.
References
- Itoi E, Yuji Hatakeyama, Takeshi Sato, Tadato Kido, Hiroshi Minagawa, et al. (2007) Immobilization in External Rotation After Shoulder Dislocation Reduces the Risk of Recurrence. A Randomized Control Trial J Bone Surg Am 89: 2124-2131.
- Taskoparan H, Volkan Kılınçoğlu, Servet Tunay, Serkan Bilgiç, Yüksel Yurttaş, et al. (2010) Immobilization of the shoulder in external rotation for prevention of recurrence in acute anterior dislocation. Acta Orthop Traumatol Turc 44(4): 278-284.
- Liavaag S, Jens Ivar Brox, Are Hugo Pripp, Martine Enger, Lars Atle Soldal, et al. (2011) Immobilization in External Rotation after Primary Shoulder Dislocation Did Not Reduce the Risk of Recurrence. J Bone Joint Am 93(10): 897-904.
- Heidari K, Shadi Asadollahi, Reza Vafaee, Abbas Barfehei, Hossein Kamalifar, et al. (2014) Immobilization in external rotation combined with abduction reduces the risk of recurrence after primary anterior shoulder dislocation. J Shoulder Elbow Surg 23(6): 759-766.
- Whelan DB, Robert Litchfield, Elizabeth Wambolt, Katie N Dainty, Joint Orthopaedic Initiative for National Trials of the Shoulder (JOINTS), et al. (2014) External Rotation Immobilization for Primary Shoulder Dislocation: A Randomized Control Trial. Clin Orthop Relat Res 472(8): 2380-2386.
- Chan S, Kieran R Bentick, Jan H Kuiper, Cormac P Kelly (2019) External rotation bracing for first-time anterior shoulder dislocation of the shoulder: A discontinued randomized controlled trial comparing external rotation bracing with conventional sling. Shoulder & Elbow11(4): 256-264.
- Murray J-C, Alexandre Leclerc, Amerigo Balatri, Stéphane Pelet et al. (2018) Immobilization in external rotation after primary shoulder dislocation reduces the risk of recurrence in young patients. A randomized control trial. Orthop Traumatol Surg Res 106(12): 217-222.
- Shinagawa K, Yumi Sugawara, Taku Hatta, Nobuyuki Yamamoto, et al. (2020) Immobilization in External Rotation Reduces the Risk of Recurrence After Primary Anterior Shoulder Dislocation. A Meta-analysis. The Orthopedic Journal of Sports Medicine 8(6): 2325967120925694.
- Akcimen M, Cihan Bedel (2020) Comparison between now modified external rotation method and external rotation method for reduction of ASD. American Journal of Emergency Medicine 38(5): 874-878.
- Bliven KH, Hamstra-Wright KL (2012) Effectiveness of External-Rotation Immobilization After Initial Shoulder Dislocation in Reducing Recurrence Rates. Journal of Sport Rehabilitation 21(2): 199-203.
- Brownson P, Michael Fox, Jonathan L Rees, Amar Rangan, Anju Jaggi, et al. (2015) BESS/ BOA Patient Care Pathways Traumatic anterior shoulder instability. Shoulder & Elbow 7(3):214-226.
- Cui X, Long Liang, Hongyan Zhang, Jing Zhao, Yongyao Li, et al. (2019) Immobilization in external rotation vs internal rotation after shoulder dislocation. A systematic review and meta-analysis protocol. Medicine. 2019;98(32): e16707.
- Gaballah, Mohamed Zeyada, Adham Elgeidi, Eadric Bressel A (2017) Six-week physical rehabilitation protocol for anterior shoulder dislocation in athletes. Journal of Exercise and Rehabilitation13(3): 353-358.
- Gutwoska O, Jacek Martynkiewicz, Jerzy Gosk (2017) Position of Immobilization After First Time Traumatic Anterior Glenohumeral Dislocation: A Literature Review. Med Sci Monit 23: 3437-3445.
- Hasebroock AW, Joseph Brinkman, Lukas Foster, Joseph P Bowens (2019) Management of primary anterior shoulder dislocations: a narrative review. Sports Medicine-Open 5(1): p. 31.
- Hutyra CA, Stephen Smiley, Dean C Taylor, Lori A Orlando, Richard C Mather 3rd, et al. (2019) Efficacy of a Preference-Based Decision Tool on Treatment Decisions for a First-Time Anterior Shoulder Dislocation: A Randomized Controlled Trial of At-Risk Patients. Medical Decision Making 39(3): 253-263.
- Itoi E, Toshio Kitamura, Shin Hitachi, Taku Hatta, Nobuyuki Yamamoto, et al. (2015) Arm Abduction Provides a Better Reduction of the Bankart Lesion During Immobilization in External Rotation After an Initial Shoulder Dislocation. The American Journal of Sports Medicine 43(7): 1731-1736.
- Jakobsen BW, Hans Viggo Johannsen, Peter Suder, Jens Ole Søjbjerg, et al. (2007) Primary Repair versus Conservative Treatment of First-Time Traumatic Anterior Dislocation of the Shoulder: A Randomized Study with 10-Year Follow-up. The Journal of Arthroscopic and Related Surgery 23(2): 118-123.
- Khiami F, Gérometta A, Loriaut P (2015) Management of recent first-time anterior shoulder dislocations. Orthopedics & Traumatology: Surgery & Research 101(1): S51-S57.
- Lacy K, Chris Cooke, Pat Cooke, Justin Schupbach, Rahul Vaidya, et al. (2015) Low-Cost Alternative External Rotation Shoulder Brace and Review of Treatment in Acute Shoulder Dislocation. Western Journal of Emergency Medicine 16(1): 114-120.
- Liu A, Xinghe Xue, Yunlin Chen, Fanggang Bi, Shigui Yan, et al. (2014) The external rotation immobilisation does not reduce recurrence rates or improve quality of life after primary anterior shoulder dislocation: A systematic review and meta-analysis. Injury Int. Care Injured 45(12): 1842-1847.
- Longo UM, Mattia Loppini, Giacomo Rizzello, Mauro Ciuffreda, Nicola Maffulli, et al. (2014) Management of Primary Acute Anterior Shoulder Dislocation: Systematic Review and Quantitative Synthesis. The Journal of Arthroscopic and Related Surgery 30(4):506-552.
- Momenzadeh OR, Masoome Pourmokhtari, Sepideh Sefidbakht, Amir Reza Vosoughi (2015) Does the position of shoulder immobilization after reduced anterior glenohumeral dislocation affect coaptation of a Bankart lesion? An arthrographic comparison. J Orthoped Traumatol 16(4): 317-321.
- Paterson WH, Thomas W Throckmorton, Michael Koester, Frederick M Azar, John E Kuhn (2010) Position and Duration of Immobilization After Primary Anterior Shoulder Dislocation: A Systematic Review and Meta-Analysis of the Literature. J Bone Joint Surg Am 92: 2924-2933.
- Prada C, Bhandari M (2019) Cochrane in CORR®: Conservative Management Following Closed Reduction of Traumatic Anterior Shoulder Dislocation of The Shoulder. Clin Orthop Relat Res 477: 1984-1990.
- Eshoj HR, Sten Rasmussen, Lars Henrik Frich, Inge Hvass, Robin Christensen, et al. (2020) Neuromuscular Exercises Improve Shoulder Function More Than Standard Care Exercises in Patients with a Traumatic Anterior Shoulder Dislocation. The Orthopaedic Journal of Sports Medicine 8(1): 1-12.
- Scheibel M, Anika Kuke, Constanze Nikulka, Petra Magosch, Ottfried Ziesler, et al. (2009) How Long Should Acute Anterior Dislocations of the Shoulder Be Immobilized in External Rotation?. The American Journal of Sports Medicine 37(7):1309-1316.
- Scheibel M, Anika Kuke, Constanze Nikulka, Petra Magosch, Ottfried Ziesler, et al. (2009) How Long Should Acute Anterior Dislocations of the Shoulder Be Immobilized in External Rotation?. The American Journal of Sports Medicine 37(7):1309-1316.
- Smith BI, Kellie C Huxel Bliven, Genoveffa R Morway, Jason G Hurbanek (2015) Management of Primary Anterior Shoulder Dislocations Using Immobilization. Journal of Athletic Training 50(5): 550-552.
- Vavken P, Patrick Sadoghi, Julia Quidde, Robert Lucas, Ruth Delaney, et al. (2013) Immobilization in internal or external rotation does not change reccurence rates after traumatic anterior shoulder dislocation. J Shoulder Elbow Surg 23(1): 13-19.
- Whelan DB, Stephanie N Kletke, Geoffrey Schemitsch, Jaskarndip Chahal (2018) Immobilization in External Rotation Versus Internal Rotation After Primary Anterior Shoulder Dislocation. The American Journal of Sports Medicine 44(2): 521-532.
- Siegler J, J Proust, P S M Marcheix, J L Charissoux, C Mabit, et al. (2010) Is external rotation the correct immobilisation for acute shoulder dislocation? An MRI Study. Orthopedics & Traumatology: Surgery & Research 96: 329-333.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...